- Coordination of benefits is the process that determines the order in which multiple insurance plans pay, ensuring there’s no duplication of payments and that claims don’t exceed the total allowed expenses
- Typically, the plan where you are an active employee is considered primary, while any plan covering you as a dependent is secondary
- For children, the coordination of benefits birthday rule is used to decide which parent’s plan is primary
- Proper coordination maximizes reimbursements, minimizes out-of-pocket expenses, and streamlines the claims process
- Administrative complexities and communication gaps between insurers can delay or complicate claim processing
- What does coordination of benefits mean?
- What are the coordination of benefits rules in Canada?
- How does coordination of benefits work?
- How to calculate coordination of benefits claims?
- Advantages of coordination of benefits
- Challenges with coordination of benefits in Canada
- How to coordinate benefits with my spouse?
- How can employers streamline coordination of benefits rules for their employees?
- Maximizing value in group benefits coordination
- Frequently asked questions
A comprehensive group benefits plan typically covers not just an employee but also their dependents. In families with two or more working adults, it is common to have more than one group health and dental insurance plan. So when a claim has to be made, which plan pays first and how are the benefits calculated? Coordination of benefits is a process that helps you understand how multiple coverages work.
This guide explains what coordination of benefits is, how it works in Canada, and what are its advantages and challenges.
What does coordination of benefits mean?
Coordination of benefits (COB) determines the order in which multiple group health insurance plans pay for a single claim. When you are covered under more than one plan, and have to make a claim, coordination of benefits ensures that:
- The primary plan pays first
- The secondary plan covers any remaining expenses
- Duplicate payments are avoided
The Canadian Life and Health Insurance Association (CLHIA) has laid down a specific order in which benefits are coordinated. All Canadian group insurance companies follow the CLHIA guidelines for coordination of benefits.
What are the coordination of benefits rules in Canada?
There are three rules that every insurance company follows when it comes to coordinating group benefits—primary vs secondary plan coverage, the birthday rule, and duration of coverage.
Primary vs secondary plan coverage for benefits coordination
Typically, the insurance plan that you get from your employer (primary plan) pays first when you make a claim for yourself. This means that if your employer has offered a group health plan to you and you are also covered under your spouse’s plan (secondary plan), your own plan will pay first.
If your healthcare claim exceeds the coverage limit of your primary plan, the secondary plan will come into effect to take care of the excess expense.
Coordination of benefits birthday rule
If your children are covered under both your and your spouse’s plan, the primary plan is determined by the birthday rule in coordination of benefits. The plan of the parent whose birthday falls first in a calendar year, is considered to be the primary plan.
This rule gets a little complicated in cases where the parents share the same birthday, in cases where the parents are separated, and with different provincial regulations. The following table gives a clearer picture of how coordination of benefits work for dependent children.
| Scenario | Claim Submission Order |
| Where both parents share the same birthday | The alphabetical order of their first names decides which plan the claim is submitted to first. The year of birth isn’t considered
For instance, if both parents were born on July 8, and the mother’s name is Francesca while the father’s name is Luke, claims should be submitted to the mother’s plan first. |
| Where the parents are separated and have shared custody of your children. If you both remarry and your children are covered under four different plans |
|
| Where you’re separated and have sole custody of your children |
|
Duration of coverage
If standard CLHIA coordination of benefits rules don’t apply, the plan that has been active for the longest duration is considered to be the primary plan. This is especially true if you work more than one job and both offer group benefits. The plan that your first employer offers will be the primary plan.
How does coordination of benefits work?
Coordination of Benefits (COB) begins with an understanding of the claim submission rules. Your first claim will be to the primary plan and any remaining amount will be covered by the secondary plan. Once your claim submission is done in the right order as laid down by your insurer, your reimbursement will be processes
Here’s how coordination of benefits work in Canada:
- Submit a claim: When you have multiple insurance plans, start by submitting your claim to your primary insurance provider
- Primary coverage: Your primary insurance provider processes the claim and pays according to your coverage and benefits
- Explanation of Benefits (EOB): Once processed, you’ll receive an Explanation of Benefits (EOB) statement detailing what was covered and what wasn’t
- Check for remaining amounts: If there are any expenses left that your primary insurance didn’t cover, you can then submit a claim to your secondary insurance provider
- Secondary coverage: Your secondary insurance provider reviews the claim and pays out based on their coverage, taking into account what your primary insurance already covered
- Reimbursement: You’ll receive reimbursement from your secondary insurance for any eligible remaining amounts, ensuring that you’re not overpaid for your expenses
What is an EOB statement?
An EOB, or Explanation of Benefits, is a document from your insurance company that explains how they handled a claim you made for medical services. It tells you what they paid for and what you might still owe.
How to calculate coordination of benefits claims?
The plan that is supposed to pay first calculates benefits without considering duplicate coverage. This means your claim will be processed like any other claim. The second paying plan calculates benefits for each item on the claim, based on the lowest of two amounts:
- The amount it would pay if it were the first plan, or
- 100% of the eligible expenses minus what the first plan already paid
Let’s consider a situation where you have $200 in eligible expenses covered under both of your plans. The first plan imposes a $25 deductible, while the second plan has no deductible. Both plans offer an 80% reimbursement rate. Here is how the reimbursement calculations play out:
Coordination of benefits reimbursement calculation
| Your Plans | Eligible Expenses | Deductible | Reimbursement % | Calculation | Your Reimbursements |
| 1st Plan | $200 | $25 | 80% | ($200 – $25) x 80% = $140 | $140 |
| 2nd Plan | $200 | $0 | 80% | ($200 – $0) x 80% = $160 | ($200 – $140) = $60 |
| Total Reimbursement | $200 (100% of expenses incurred) |
Things to remember:
- Total payments from all plans can’t exceed 100% of the eligible medical or dental expenses
- Sometimes, the combined payments from all plans might be less than what you paid out of pocket
- Some plans limit visits to a health/dental practitioner per year (e.g., once every nine months), and some have an annual maximum dollar limit
- When a plan pays any benefit for a visit, it counts as a visit and contributes to any maximums under both plans
Advantages of coordination of benefits
A streamlined coordination of benefits process ensures maximum coverage with minimum out-of-pocket expenses. With effective coordination of benefits, you can get almost 100% of your claims reimbursed for eligible medical expenses.
For instance, if you need an MRI and your primary plan covers 60% of the cost, your secondary plan will most likely cover the rest. This significantly reduces your out-of-pocket costs for medical expenses.
A clear coordination of benefits process also helps in settling claims faster, benefitting both employees and employers.
Challenges with coordination of benefits in Canada
Coordination of benefits in Canada can be administratively challenging, especially if the guidelines are not understood clearly.
- Administrative and implementation challenges: The rules that multiple insurers lay down for coordinating benefits can be hard to understand. Incomplete or inaccurate information during the claims process can lead to delays, especially if the documentation is submitted in an incorrect order
- Provincial variation in COB rules: Some provinces such as Quebec have different coordination of benefits rules. For instance, if your child is covered under a work plan, a student plan, and your plan, insurers in Quebec will consider the work plan as the primary coverage, and yours as secondary. This is unlike the rest of Canada where the student plan is the primary coverage
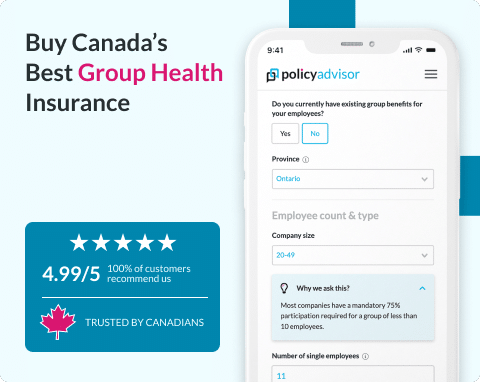
At PolicyAdvisor, our after-sales service includes supporting you and your employees to make claims in a way that maximizes the chances of approval. Speak to one of our experts today and get an affordable group benefits plan for your organization.
How to coordinate benefits with my spouse?
To effectively coordinate benefits with your spouse, you will have to determine the primary and secondary plans that you are covered under along with the birthday rule. Here are a few key things to remember when coordinating benefits with your spouse:
- The plan your employer offers is always going to be the primary plan and will pay first
- Any excess expense that your plan does not cover, can be covered by your spouse’s plan
- For your dependent children, the primary plan will be of the parent whose birthday falls first in a calendar year
- If you and your spouse share a birthday, the alphabetical order of your names will determine the primary and secondary plan
How can employers streamline coordination of benefits rules for their employees?
Employers can communicate coordination of benefits rules to their employees on a regular basis, ensure claims are handled efficiently with the insurer, and simplify documentation processes.
- Effective communication: Ensure your employees have clear and accessible information on how coordination of benefits work within your organization
- Claims management: Work with your insurer to streamline the claims process
- Simplify documentation: Find an insurer that uses digital tools and processes that help employees submit and track claims
Maximizing value in group benefits coordination
Employers can ensure their employees get maximum value by effectively coordinating their benefits with that of their common law partners or spouses. Identifying an insurer that offers group benefits with a streamlined coordination process is the first step towards achieving this goal.
At PolicyAdvisor, we work with top Canadian insurers offering group benefits with advanced tools and streamlined processes that make claims submissions easy for employees. Our AI calculator can help you identify an affordable employee benefits package from over 30 of Canada’s insurance providers. Compare prices and make a choice in just a few minutes!
Want personalized help? Book a no-obligation call with one of our licensed group health insurance experts today!
Frequently asked questions
What happens if both plans don’t cover the full amount?
If both the primary and secondary plan don’t cover the full amount of your healthcare expense, you will typically have to pay out-of-your-own-pocket. Regardless of being covered under multiple plans, the total coverage amount cannot exceed 100% of the medical expense. In addition, deductibles and copays will have to be paid by you.
Can I coordinate benefits with a plan from a previous employer?
You can coordinate benefits with a plan from a previous employer provided the coverage is still active. Group benefits are generally not portable, they end with your employment. However, in some cases, the group benefits have a grace period—they continue for about 30-60 days after employment ends. If you get another plan during this period, you can make claims on both, starting with your new employer’s plan.
How do I update my coordination of benefits information?
To update any information that will affect how your benefits are coordinated, you will need to speak to your insurer or your company’s administrator. Information such as adding a dependent child, change in marital status, etc. should be immediately notified to ensure your benefits are effectively coordinated.
Some insurers may require you to fill out specific forms. It is crucial that you check your policy document for the same.
Are there exceptions to typical coordination rules?
Yes, there are exceptions to the typical coordination of benefits (COB) rules in Canada. While the standard approach is that the employee’s plan pays first, followed by the spouse’s, certain situations require different rules.
For example, when parents are divorced or separated, the plan of the parent with primary custody usually pays first. If custody is shared, the birthday rule may still apply. Coordination also works differently between public and private plans; provincial health coverage always pays first, but COB typically applies only between private plans.
In cases involving emergency medical care abroad, travel insurance provisions may override normal coordination rules. Additionally, some plans include non-duplication clauses, meaning they won’t pay if another plan already covers the full amount.
When employees or dependents have coverage under more than one group benefits plan, Coordination of benefits (COB) determines the order of payment to avoid duplicate reimbursements and maximize coverage. Understanding which plan pays first—whether for employees, dependents, or unique family situations (e.g., divorced or remarried parents)—ensures smooth claim processing. Employees should first submit claims to their primary plan, wait for an Explanation of Benefits (EOB), then forward it to the secondary plan for any remaining eligible expenses. When used effectively, COB can significantly reduce healthcare expenses for employees and their families, ensuring better financial protection.

 1-888-601-9980
1-888-601-9980